
The executives examined independent market research that surveyed health plan leaders about the current state of UM and what organizations need to transform both Utilization Management and Care Management.
Key findings relative to UM include:
- More than half of survey respondents say fragmented data (57%), data that doesn’t flow into UM workflows (55%), and burdensome data integration are the top barriers to current tools
- 68% say inefficient workflows are their organization’s primary frustration with current tools, followed by high costs associated with data silos (49%), and provider abrasion (40%)
- Why? Because respondents say current tools are not easy to use and they need technologies that are “very effective” at accessing real-time data to drive down administrative and medical costs while improving health outcomes
In addition to sharing the research, the speakers also discussed:
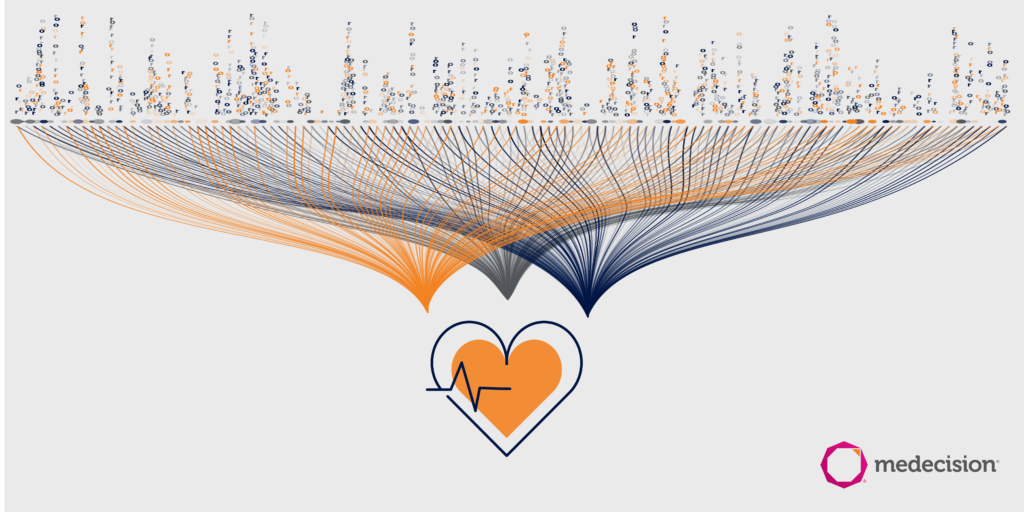
- Data types healthcare organizations should be integrating into UM workflows
- The power of personalization in making UM more trusted by members and providers
- How predictive modeling for risk stratification, as well as UM workflow optimization with AI and automation, can propel UM efficiency, results, and outcomes
- What leaders should understand about regulations relative to UM – including the newly-released ePrior Authorization rule


About The Author: Medecision
Medecision is a leader in cloud-based, data-powered healthcare solutions, enabling risk-bearing entities to achieve improved health outcomes, optimized medical costs, reduced administrative costs, and personalized engagement. Our Aerial platform supports over 10% of the U.S. population, marking a significant milestone in advancing healthcare efficiency and effectiveness.
More posts by Medecision