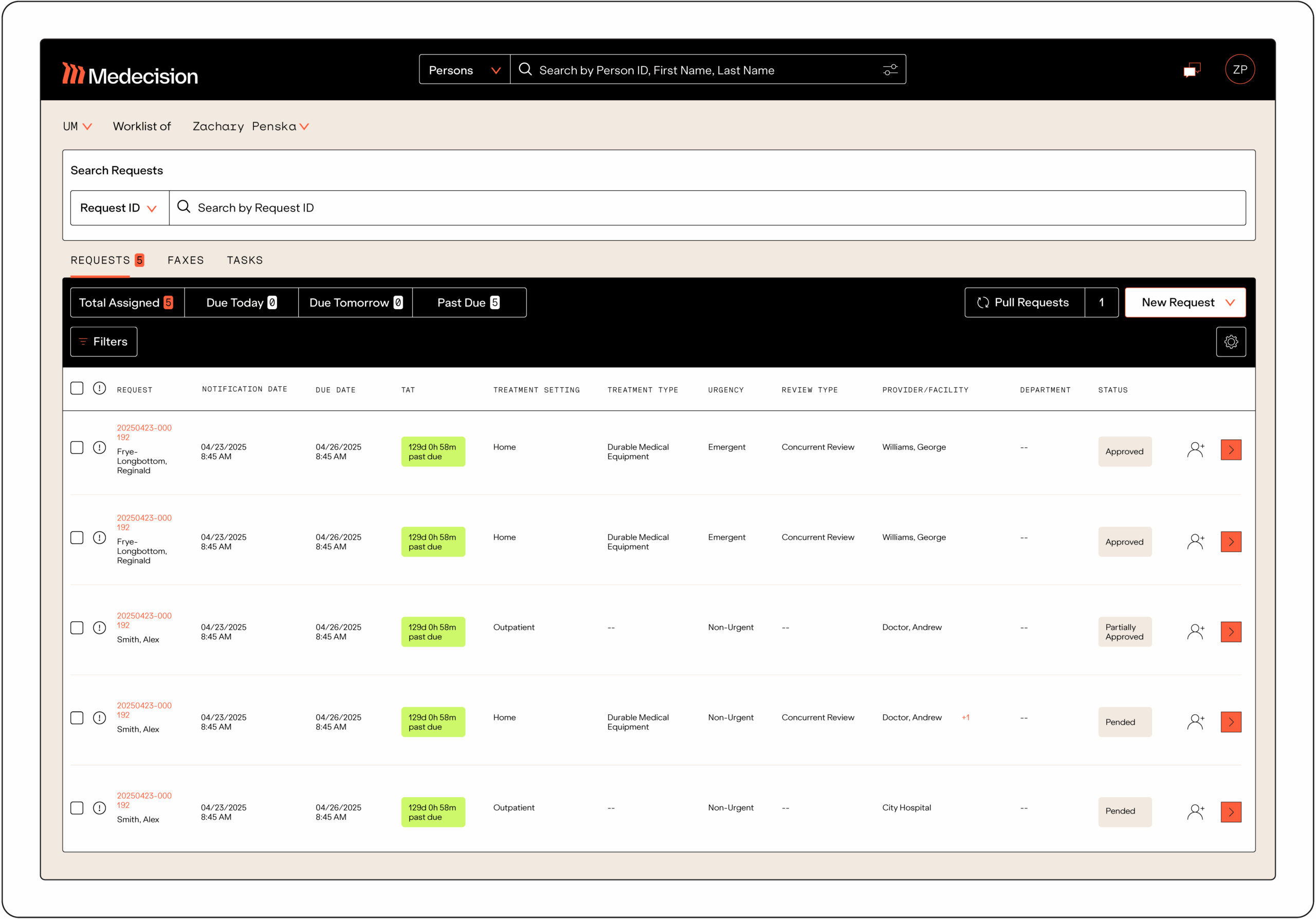
I’ve enjoyed working with the Medecision team since 2003. They’re very professional, knowledgeable and energetic. They inspire me to go the extra mile, to work harder. We started years ago with utilization management workflow, administration and reporting. By listening to customer feedback, Medecision has a positive impact on healthcare. Its solutions and services continue to help us achieve our vision of building a healthier, happier Hawaii.”
Guy Ng
Senior Utilization Management Solutions Analyst
Hawaii Medical Service Association