
A game-changing revision to CMS rules for Star ratings puts Medicare Advantage plans under extra pressure to deliver an excellent customer experience. At Medecision, our solutions and services help health plans improve the consumer experience and increase engagement.
By Medecision
There’s a growing emphasis on consumer experience across industries, and healthcare is no exception. In fact, it could be argued that a positive consumer experience is never more important than when someone’s health—physical, mental or both—is at stake.
A May 2020 revision by the Centers for Medicare & Medicaid Services (CMS) to the Star Ratings system puts Medicare Advantage (MA) plans under extra pressure to deliver an excellent customer experience, with potentially billions of dollars on the line. By shifting the emphasis from individual measures to patient/member experience, engagement and satisfaction measures, CMS made the rating more dependent on experience measures where the healthcare industry has long struggled to improve. As a result, industry analysts expect Star performance to decline—at least until MA plans figure out how to meet consumer experience expectations, the most challenging set of metrics to satisfy.
Why This Revision Is a Game Changer
Medicare Advantage, also known as “Part C” plans, are offered by Medicare-approved private companies as an alternative way for consumers to obtain coverage. Participating companies must meet performance thresholds to achieve incentive payments established by Medicare, and for many the MA plans represent their fastest-growing line of business.
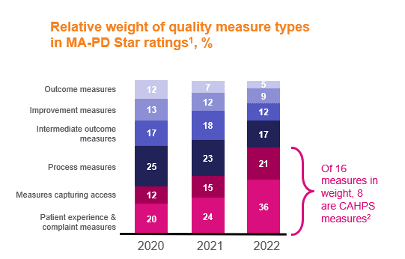
CAHPS, Consumer Assessment of Healthcare Providers and Systems; MA-PD, Medicare Advantage prescription drug plan
1 Figures may not sum to 100% because of rounding
2 Excluding duplicative measures for Part C and Part D ratings
Under the new methodology for calculating MA quality scores, consumer experience-related metrics will determine 57% of overall Star ratings by 2023. That’s an increase of 25 percentage points! Even before this change, customer experience measures had been part of the Star equation for years, “with roughly $15.1 billion in Stars-linked incentives creating a performance imperative,” McKinsey & Company’s Stephanie Carlton, David Malfara, Kevin Neher and Cara Repasky reported last year in “New Stars Ratings for Medicare Advantage Prioritize Customer Experiences.”
This heightened emphasis clearly ups the ante, as “health plans have not been as successful in improving their customer experience as other industries,” the McKinsey team wrote. Its report cites case studies from the banking and pharmaceuticals industries to show how data- and analytics-driven approaches to improving the customer experience have generated tens of millions of dollars in additional revenue.
Conversely, because of the increased weight of customer experience measures, a company’s revenue could decline even if actual performance on those metrics was unchanged.
Why You Need to Look Holistically at Your Programs and Consumer Experience
Star ratings are publicly available on websites such as Medicare.gov and Healthcare.gov, along with state-specific health information exchange sites. Medicare’s website also allows members to compare nursing homes, hospitals, dialysis centers and other providers. This public information makes it critically important for plans to focus on improving their Star ratings in order to attract and retain members.
“Excellent customer experiences will be even more critical moving forward,” the McKinsey team wrote. “An analytics-driven approach to customer experience redesign could ensure Star performance, while potentially driving growth for plans. Additionally, it could materially (improve) seniors’ experience with healthcare.”
The report concludes: “To achieve high Star ratings—and more broadly drive growth—MA plans will need to adjust their mindsets from a focus on gap closure to a holistic view of the member experience. Advanced analytics can sharpen this view and help identify the most impactful interventions. Customer experience investments can improve Stars performance and health plan economics, but they also present a way to improve the member experience of a complex and often frustrating healthcare system at a time when healthcare has never mattered more.”
Aveus, the professional services and strategic consulting division of Medecision, has experience in helping health plans improve their Star ratings and patient experience ratings.
Achieving improvements in experience that support improved Star ratings requires focus and partnership. When Aveus begins this work with a client, they conduct internal stakeholder interviews, data analysis and ideal experience mapping with a cross-functional team. In addition, Aveus shares recommendations for improving the member experience and best practices from other health plans with 5-Star ratings, such as:
- Building a success-oriented culture, with strong executive support and regular communication
- Speaking like members, using consumer language that helps members connect plan benefits to the way they live their life
- Engaging providers by treating them like partners and incentivizing them around desired patient experience metrics
- Managing the network, getting more control over experience and ratings results
- Committing to improving the patient experience with proactive outreach
Subsequent work moves the recommendations into action and focuses on establishing an end-to-end member experience strategy and working on proactive outreach strategies to members. Additional support focuses on implementation of recommended changes, helping the client develop a culture change plan and operational roadmap.
In addition, trust is an essential piece of the patient/consumer experience, as we’ve written before in this space. In order to meet and exceed consumer expectations, organizations must learn all they can about the whole patient—which is not possible without first earning their trust. Similarly, organizations must be able to trust their partners in meeting this challenge.
Do you have a trusted partner in your quest to improve the consumer experience? If not, reach out to Medecision and Aveus; we welcome the opportunity to earn your trust.
Editor’s Note: On August 5, 2021, CMS announced that two Health Outcomes Survey (HOS) outcome measures, Improving or Maintaining Physical Health and Improving or Maintaining Mental Health, will be removed from 2022 and 2023 calculations due to COVID-19. Learn more here and here.


About The Author: Medecision
Medecision is a leader in cloud-based, data-powered healthcare solutions, enabling risk-bearing entities to achieve improved health outcomes, optimized medical costs, reduced administrative costs, and personalized engagement. Our Aerial platform supports over 10% of the U.S. population, marking a significant milestone in advancing healthcare efficiency and effectiveness.
More posts by Medecision